Connect with BioMarin
Register to get Brineura updates, as well as helpful resources and information.
The safety of Brineura® (cerliponase alfa) was evaluated in 24 patients with CLN2 disease who received at least 1 dose of Brineura in a clinical study with extension of up to 161 weeks.1
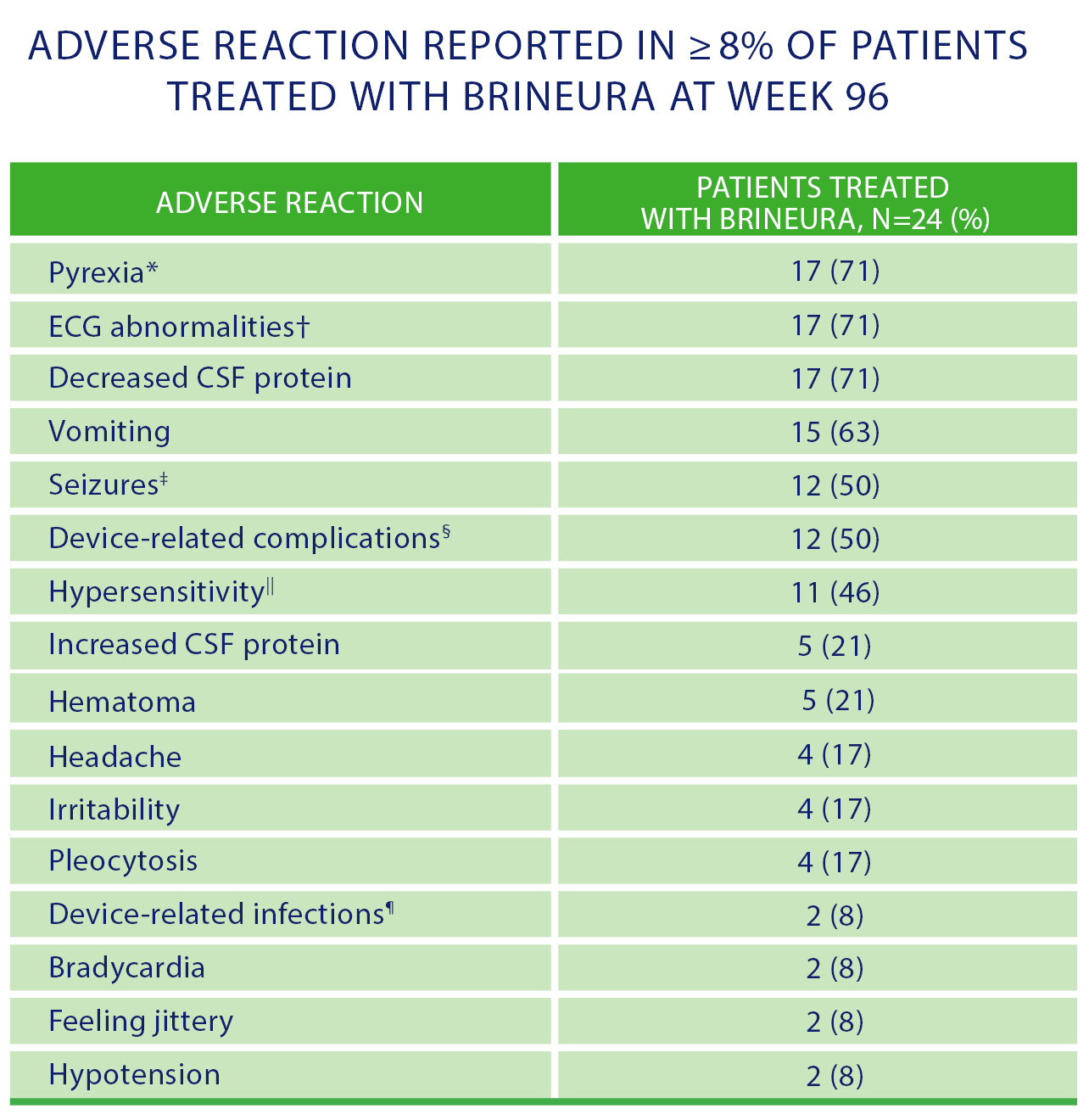
* Pyrexia includes pyrexia and increased body temperature.
† ECG abnormalities include nonspecific repolarization abnormality, notched QRS, ST segment elevation, biphasic T wave abnormality, supraventricular extrasystoles, bradycardia, sinus tachycardia, and intraventricular conduction delay.
‡ Seizures include atonic, generalized tonic-clonic, focal, and absence.
§ Device-related complications include device-related infection, delivery system related complications (needle issues, device leakage, device malfunction, device difficult to use, etc) and pleocytosis.
|| Hypersensitivity includes immune reactions and signs and symptoms observed concomitantly with hypersensitivity reactions including pyrexia, vomiting, pleocytosis, or irritability.
¶ Device-related infections include Propionibacterium acnes and Staphylococcus epidermidis.
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
Due to the potential for anaphylaxis, appropriate medical support should be readily available, and patients should be observed closely, during and after Brineura infusion. If anaphylaxis occurs, immediately discontinue infusion and initiate appropriate medical treatment. Inform patients/caregivers of the signs and symptoms of anaphylaxis and to seek immediate medical care should these occur. Consider the risks and benefits of readministration of Brineura following an anaphylactic reaction.
To report suspected adverse reactions, contact:
BioMarin Pharmaceutical Inc.
Phone: 1-866-906-6100
Email: drugsafety@bmrn.com
FDA
Phone: 1-800-FDA-1088
Web: www.fda.gov/medwatch
For medical information inquiries:
BioMarin Medical department
Email: medinfo@bmrn.com
Phone: 1-800-983-4587
Fax: 1-866-524-0038
IMPORTANT SAFETY INFORMATION
Contraindications
Brineura is contraindicated in patients with:
Important Preparation and Administration Information
Brineura must only be administered via the intraventricular route using aseptic technique to reduce the risk of infection. Administer Brineura and the Intraventricular Electrolytes using the provided Administration Kit for use with Brineura components. Prior to each infusion, inspect the scalp for signs of intraventricular access device leakage or failure and for potential infection. Prior to each infusion of Brineura and when clinically indicated, send cerebrospinal fluid (CSF) samples for testing of cell count and culture.
Special Populations
Brineura has not been studied in pregnancy or lactation.
Safety and effectiveness in pediatric patients below 3 years of age have not been established.
WARNINGS AND PRECAUTIONS
Meningitis and Other Intraventricular Access Device-Related Infections
Bacterial meningitis requiring antibiotic treatment and removal of the device was reported during postmarketing use of Brineura. The signs and symptoms of infections may not be readily apparent in patients with CLN2 disease. To reduce the risk of infectious complications, Brineura should be administered by, or under the direction of, a physician experienced in intraventricular administration.
Intraventricular Access Device-Related Complications
During the clinical trial and in postmarketing reports, intraventricular access device-related complications were reported (e.g., device leakage, device failure, extravasation of CSF fluid, or bulging of the scalp around or above the intraventricular access device). In case of intraventricular access device-related complications, discontinue the Brineura infusion and refer to the device manufacturer’s labeling for further instructions.
Material degradation of the intraventricular access device reservoir was reported after approximately 4 years of administration, which may impact the effective and safe use of the device. The intraventricular access device should be replaced prior to 4 years of single-puncture administrations, which equates to approximately 105 administrations of Brineura.
Cardiovascular Adverse Reactions
Monitor vital signs before infusion starts, periodically during infusion, and post-infusion in a healthcare setting. Perform electrocardiogram (ECG) monitoring during infusion in patients with a history of bradycardia, conduction disorder, or with structural heart disease. In patients without cardiac abnormalities, regular 12-lead ECG evaluations should be performed every 6 months.
Hypersensitivity Reactions, Including Anaphylaxis
Hypersensitivity reactions, including anaphylaxis, have been reported in Brineura-treated patients during clinical studies and postmarketing use. In clinical trials, a total of 11 out of 24 patients (46%) experienced hypersensitivity reactions during the infusion or within 24 hours of completion of the infusion.
Due to the potential for anaphylaxis, appropriate medical support should be readily available when Brineura is administered. If a severe hypersensitivity reaction or anaphylaxis occurs, immediately discontinue the infusion and initiate appropriate medical treatment. Observe patients closely during and after the infusion. Inform patients/caregivers of the signs and symptoms of hypersensitivity reactions and anaphylaxis and instruct them to seek immediate medical care should signs and symptoms occur. Consider the risks and benefits of readministration of Brineura following an anaphylactic reaction.
ADVERSE REACTIONS
In clinical trials, the most frequently reported adverse reactions (≥8%) were pyrexia, ECG abnormalities, decreased CSF protein, vomiting, seizures, device-related complications, hypersensitivity, increased CSF protein, hematoma, headache, irritability, pleocytosis, device-related infection, bradycardia, feeling jittery, and hypotension.
Seizures were reported in 12 of 24 patients and included atonic, generalized tonic-clonic, focal, and absence. Seizures were managed with standard anticonvulsive therapies and did not result in discontinuation of Brineura treatment.
Adverse reactions related to the device were observed in 12 of 24 patients. Device-related adverse reactions include infection, delivery system-related complications, and pleocytosis.
Hematoma adverse reactions were reported in 5 patients and presented as hematoma, post-procedural hematoma, traumatic hematoma, and subdural hematoma. Hematomas did not require treatment and did not interfere with Brineura infusion.
Anti-drug antibodies (ADAs) were detected in serum (79%) and CSF (33%) in patients treated with Brineura. No association was found between serum or CSF ADA titers and incidence or severity of hypersensitivity.
To report SUSPECTED ADVERSE REACTIONS, contact BioMarin Pharmaceutical Inc. at 1-866-906-6100, or FDA at 1-800-FDA-1088, or go to www.fda.gov/medwatch.
Please see accompanying full Prescribing Information, or visit www.Brineura.com.
INDICATION
Brineura® (cerliponase alfa) injection for intraventricular use is indicated to slow the loss of ambulation in symptomatic pediatric patients 3 years of age and older with late infantile neuronal ceroid lipofuscinosis type 2 (CLN2), also known as tripeptidyl peptidase 1 (TPP1) deficiency.